Handoffs and Transitions of Care: A Systematic Review, Meta-Analysis, and Practice Management Guideline from the Eastern Association for the Surgery of Trauma
Published 2024
Citation: Journal of Trauma and Acute Care Surgery:10.1097/TA.0000000000004285, February 26, 2024
Authors
Rachel D. Appelbaum, MD; Thaddeus J. Puzio, MD, FACS; Zachary Bauman, DO, MHA, FACOS, FACS; Sofya Asfaw, MD; Audrey Spencer, MD; Ryan P. Dumas, MD, FACS; Kavneet Kaur, BS; Kyle W. Cunningham, MD, MPH, FACS; Dale Butler, MD, MBA; Jaswin S. Sawhney, MD; Stephen Gadomski, MD; Chelsea R. Horwood, MD, MPH; Mary Stuever, DO; Alyssa Sapp, MLIS, AHIP; Rajesh Gandhi, MD, PhD, FACS, FCCM; Jennifer Freeman, MD, MPH, FACS
Introduction
The “handoff” is an essential component of modern healthcare practice where the transmission of patient-specific information occurs between providers to maintain continuity of care. In the early 2000s, the Joint Commission and the Institute of Medicine identified communication failure as a key root cause of preventable adverse events in medicine [1][2]. In a study of deaths in Level I trauma centers, human and system errors were responsible for 10% of preventable mortalities [3]. Errors in communication are particularly common during the transition of care for a patient’s initial presentation, to and from the operating room (OR), and on arrival to the intensive care unit (ICU) or floor. Passive listening, perceived disinterest in the receiving staff, competing interests (such as the ongoing resuscitation of the patient), non-standardized transfer tools, and interruptions are some of the barriers to effective communication during these critical time points that have been previously identified in the literature [4-6].
To combat this poor communication, several institutions have reported on their efforts to standardize the handoff process. A standardized handoff often includes a synopsis of the patient’s baseline characteristics and important comorbidities, a reason for admission, a short summary of current hospital course, current active issues, and next steps involved in the patient’s care which may include active items to complete or follow-up on. Evidence-based recommendations on the use of a standardized or formal handoff process in the field of Acute Care Surgery (ACS), which includes Trauma, Emergency General Surgery, and Surgical Critical Care, is lacking. We performed a systematic review and meta-analysis to develop evidence-based recommendations on the utility of a standardized handoff in Acute Care Surgery. We specifically evaluated handoffs during perioperative interactions and the management of patients arriving to the trauma bay, or transitioning within/between the floor or ICU, to reduce clinical complications, handoff errors, medical errors, and preventable adverse events utilizing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology.
Objectives
This guideline was developed by assembling a working group of members of the Eastern Association for the Surgery of Trauma (EAST) Guidelines Committee, with the plan to conduct a formal systematic literature search and review, per the GRADE methodology [7]. The working group consisted of EAST members and non-EAST members with expertise in ACS. Population, Intervention and Comparison (PIC) stems were developed after consensus.
The following PIC and Outcome (PICO) questions were formulated:
PICO 1
In the setting of ACS, specifically perioperative interactions (P), should a standardized handoff be performed (I) versus the currently established process (C) to help reduce clinical complications, the rate of handoff errors, the rate of medical errors, and preventable adverse events (O)?
PICO 2
In the setting of ACS, specifically EMS and trauma team interactions (P), should a standardized handoff be performed (I) versus the currently established process (C) to help reduce clinical complications, the rate of handoff errors, the rate of medical errors, and preventable adverse events (O)?
PICO 3
In the setting of ACS, specifically intra/inter floor and ICU interactions (P), should a standardized handoff be performed (I) versus the currently established process (C) to help reduce clinical complications, the rate of handoff errors, the rate of medical errors, and preventable adverse events (O)?
As mentioned, we aim to evaluate the utility of standardization vs no standardization in ACS handoffs. The comparator “current process ” refers to the handoff process in place prior to implementation of the standardized process as part of the study.
Methods
Identification of References
Our systematic review was registered with PROSPERO (registration No CRD42021262929). Medline via , Embase, Cochrane Central Registry Controlled Trials, and the Web of Science were searched on the topic between 1960 and 2021, search strategy available in Supplemental Digital Content 2, Table 1, http://links.lww.com/TA/D585, on July 6, 2021 by a professional librarian (AS) at Texas Christian University. Only published observational and randomized studies that included both patients receiving the intervention and comparator were eligible for review. Case series, case reports, commentaries, animal studies, and operative technique articles were excluded. Reviews were assessed to ensure their referenced primary studies were included in our results. Only studies in English were included.
Selection of Outcomes
In accordance with the GRADE approach, numerous candidate outcomes were considered and these were voted independently by each author on a scale from 1 to 9 for each PIC stem. Outcomes with scores 7-9 were considered critical and included in our analysis, those with scores 4-6 important, and those with scores in the 1-3 range of limited importance. The outcomes considered and their rounded means are summarized on Supplemental Digital Content 2, Table 2, http://links.lww.com/TA/D585. Perioperative interactions are defined as all communication occurring pre-, intra-, or post- operatively regarding the handoff or transition of care of Acute Care Surgery patients. Intra-/inter-floor interactions were defined as all handoff or transition of care communication occurring among providers on a specific floor/ICU or during the transition of a patient from a floor/ICU to another level of care. Clinical complications were defined as mortality, as no other clear clinical complication was reported. Handoff errors were defined as issues with the handoff process itself (cumulative errors) including information omissions and inability to retain the information transferred. Medical errors were defined as medical issues that did not lead to mortality, and included complications as a result of the handoff process. Preventable adverse events were defined as events not part of the expected clinical course, and a consequence of failure of the handoff process. Several studies describe re-admissions to the ICU as preventable and due to failure of the handoff process, but it is important to mention, in clinical practice, not all re-admissions to the ICU or hospital are preventable and instead are due to medical complications of the patient’s clinical course.
Data Extraction and Management
Titles, abstracts and full texts were reviewed in duplicate, independently by two separate team members, and any conflicts were adjudicated by a third. All reviews took place in Covidence, a web-based collaboration software platform that streamlines the production of systematic and other literature reviews [8]. Data were extracted also in duplicate in Excel (Microsoft, Redmond, WA) and meta-analyzed on RevMan Online [9]. Odds Ratios with 95% confidence intervals for dichotomous outcomes and differences in means with 95% confidence intervals were calculated for the intervention versus the comparison groups. Statistical significance was declared at p<0.05. Heterogeneity was calculated and quantified with I2. Low degree of heterogeneity had I2 values less than 50%. Moderate heterogeneity had I2 values of 50-74%, and ones with I2 values >75% were indicative of high heterogeneity [10]. The quality of the evidence was assessed with GRADEpro [11] taking into consideration potential risk of bias including inconsistency, indirectness, imprecision, and publication bias. Based on the results of the meta-analyses and the evidence quality, all members of the working group then voted on recommendations for each PICO question, taking additionally into consideration the relationship of benefits and harms, patient values and preferences, and resource utilization. The whole review followed strictly the GRADE methodology [7]. The PRISMA guideline was used to ensure proper reporting of methods, results, and discussion, Supplemental Digital Content 3, http://links.lww.com/TA/D586.
Results
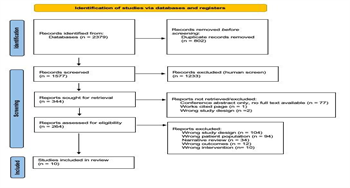
The literature search yielded 2,379 studies, of which 10 met criteria for inclusion and were fully analyzed, Figure 1 – PRISMA flow diagram. The included studies and their characteristics are summarized on Table 1.
PICO 1: Should perioperative interactions in the care of ACS patients (P) include a standardized handoff (I) versus current process without a standardized handoff (C) to help reduce clinical complications, handoff errors, medical errors, and preventable adverse events (O)?
Qualitative analysis
Five studies were included in our analysis of PICO 1. The included studies were published between 2013 and 2020 [4][12-15]. A total of 586 and 845 patients were in the intervention and comparison groups, respectively.
In 2013, Nagpal et al. performed a prospective cohort study that aimed to improve post-operative handoffs through the implementation of a new handoff protocol. The new protocol involved standardization of the process. A trained researcher observed the handoffs using a validated assessment tool [16] to evaluate the quality of the process before and after implementation. Overall, there was a significant reduction in the rate of errors (information omissions), rate of medical errors, and handoff time. Satisfaction scores also significantly improved [12].
In 2016, Salzwedel et al. performed a prospective, randomized control trial (RCT) to increase quality information transfers through the implementation of an OR to ICU checklist. Handoffs were observed, recorded, and analyzed using an individual rating sheet to compare the quality of the process with and without a formal checklist. The authors determined the information which “must” be handed over versus “should” be handed over based on provider input. More items were handed over with the implementation of a standardized handoff process, resulting in a significant decrease in the amount of missing information, 12.9% vs 25% respectively [13].
Several prospective cohort studies were performed in 2019. Faiz et al. aimed to determine whether a standardized handoff could be implemented using the “theory of change” with education, introduction of a checklist, and development of a feedback mechanism [17]. A pre-intervention assessment of handoffs was performed followed by direct observation utilizing a standardized checklist. A survey was conducted to measure perceptions and satisfaction. Overall, handoff errors significantly decreased, and at six months providers still reported improved quality of information transferred and teamwork suggesting a larger culture change [14].
The post-operative handoff is often compromised by reporting inconsistencies. Shah et al. aimed to implement a multidisciplinary quality improvement initiative to improve post-operative information reporting [4]. The authors utilized Six Sigma methodology to identify deficiencies in the existing post-operative handoff process, created a standardized process including a checklist and electronic handoff note, and then directly observed handoffs post-implementation to determine reporting accuracy, duration, and provider attendance. The rate of handoff errors (cumulative errors) significantly decreased. No difference was seen in overall handoff duration. The authors concluded that a standardized handoff process was associated with improved information reporting without significant lengthening of the transition of care.
In 2020, Lane-Fall et al. developed a prospective cohort study to assess the effectiveness of standardizing OR to ICU handoffs in a mixed surgical population. The primary outcome evaluated was the number of information omissions out of 13 possible topics. The authors found information omissions were linearly associated with the number of protocol steps and acknowledging this can lead to reduced omissions, p<0.001. The rate of handoff errors (omissions) showed a significant decrease. Of note, ICU mortality and LOS did not change post implementation; however, no further details were included on these outcomes [15]. The authors concluded standardizing OR to ICU handoffs significantly improved information exchange; however, additional research is needed to identify barriers to and facilitators of protocol adherence.
These studies demonstrate encouraging results in the perioperative setting for handoffs and transitions of care with improved communication; however, they are not without limitations and potential biases. All of the studies involved a component of observation of the handoff process and possible Hawthorne effect whereby behavior is altered by the observation process. The studies tried to minimize this by using observers not involved in the transformation process. Additionally, all of the studies involved a single institution which may affect the generalizability of the findings. The studies were pre and post-intervention designs which prevents the determination of whether institutional or environmental trends unrelated to the study drove change. Faiz et al. only had short term follow-up; long term sustainability remains to be seen. For Salzwedel et al., there was poor compliance with the checklist, 18.5% of “must include” items deemed by the providers were often omitted. [4][12-15].
Quantitative analysis
A total of 415 and 510 patients were in the intervention and comparison groups, respectively. Due to only 1 study being included for outcomes of clinical complications, the rate of medical errors, and preventable adverse events, we are unable to perform a meta-analysis for those outcomes, Table 2A.
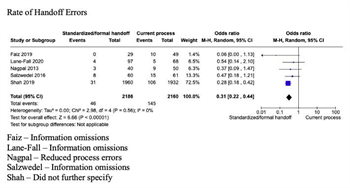
Rate of handoff errors:
The pooled data demonstrates that patients who received a standardized handoff were less likely to experience handoff errors (OR 0.31, 95% Confidence Interval 0.22-0.44, p<0.001). Heterogeneity was low (I2<50%) which suggests that chance satisfactorily provides an explanation for the variability in the individual point estimates, Figure 2A. There were only 4 publications that reported rates of handoff errors during perioperative interactions.
PICO 2: Should EMS utilize a standardized handoff at the arrival of trauma patients (I) versus current process without a standardized handoff (C) to help reduce clinical complications, handoff errors, medical errors, and preventable adverse events (O)?
Qualitative analysis
One study was included in our analysis of PICO 2. This study reported the rate of handoff errors. No studies were found that directly addressed the remaining outcomes of interest in this particular clinical setting, EMS to trauma team handoff. The included study was published in 2007 [18]. A total of 10 and 8 patients were in the intervention and comparison groups respectively.
In 2007, Talbot et al. developed a retrospective study to evaluate handoff practices within two large emergency departments, specifically looking at the EMS to ED provider transition of care. They utilized the DeMIST tool [De – Demographics; M- Mechanism of injury/illness; I – Injuries suspected or sustained; S- Signs (observation/monitoring); T – Treatment given] for verbal handoff of pre-hospital information in one of the two emergency departments. The number of packets of information in the verbal handoff and the accuracy of the communication were assessed. Pre-intervention 56.5% of the information given at verbal handoff was retained by ED whereas 49.2% was retained after DeMIST implementation, making the missed information 43.5% versus 50.8% respectively. The authors conclude communication training, clinical leadership, and team discipline must support the communication process. ED staff may have fared worse in structured handoff due to distraction of the ambulance staff trying to use the unfamiliar system. It is unclear if the ED staff was specifically trauma trained. [18].
As mentioned previously in PICO 1, this study is not without limitation and potential bias including the Hawthorne effect, extremely small sample size, and pre/post-intervention design [18].
Quantitative analysis
A total of 10 and 8 patients were in the intervention and comparison groups respectively. Due to only 1 study being included, we are unable to perform a meta-analysis.
PICO 3: Should intra/inter floor and ICU interactions in the care of ACS patients (P) include a standardized handoff (I) versus currently process without a standardized handoff (C) to help reduce clinical complications, handoff errors, medical errors, and preventable adverse events (O)?
Qualitative analysis
After literature review, four studies were included in our analysis. Two studies analyzed clinical complications. One study each was identified for the analysis of the rate of handoff and medical errors, respectively. Three studies reported preventable adverse events. The included studies were published between 2017 and 2019 [19-22]. A total of 4,807 and 4,988 patients were in the intervention and comparison groups respectively.
In 2017, Clanton et al. performed a RCT of handoffs versus focused handoffs. Residents were trained in handoff techniques and then observed by trained researchers. Focused handoffs were significantly faster and involved fewer patients. Adverse events occurred during 16.7% of patient admissions. Overall, the length of stay was shorter in the formal group, 5.88 versus 5.50 days, p=0.024 [19]. The authors concluded a minimalistic handoff process may save time and resources without negatively affecting patient outcomes.
Unreliable and incomplete handoffs of complex patients contribute to preventable ICU readmissions. In 2017, Hoffman et al. performed a prospective cohort that aimed to address care coordination surrounding the transfer of patients form the ICU to the surgical ward. Handoffs of patients discharged from the surgical ICU to the floor were observed. Process metrics and clinical outcomes were compared to historical controls. Overall, readmission rates decreased with standardization demonstrating implementation of a protocol is feasible and results in improved care coordination and communication for high risk, ICU patients [20].
Also in 2017, Wessman et al. performed a retrospective cohort study to evaluate a communication improvement project. The authors used the glass doors in the surgical ICU to fill out goals of care for each shift and updated this throughout the day. They retrospectively reviewed patient safety events in the ICU pre and post-implementation. They noted a decrease in handoff communication errors of 46.5%. The authors concluded the glass door handoff tool is an easily adaptable intervention that demonstrates improved communication leading to an overall decrease in the number of handoff errors [21].
In 2019, Stahl et al. aimed to determine how critical information degrades and is lost over 24 hours for critically ill ICU patients experiencing multiple transitions of care. An observational control period was followed by a didactic session on the science and use of a checklist as well as the implementation of a standardized handoff. The authors determined a structured checklist significantly reduces patient errors due to lost information and communication lapses between trauma ICU team members at handoffs of care [22].
As mentioned in PICO 1 and 2, these studies are not without limitations and potential biases including the Hawthorne effect. Clanton et al. notes the potential learning effects on the study outcomes. Learned elements from the standardized handoff cannot be unlearned for the focused handoff, possibly leading to crossover even with randomization of the patients. Wessman et al. notes their study may be limited by weaknesses in the self-reporting system used. Hoffman et al. had a small rate of events and the study was underpowered to detect significant differences in the clinical outcomes. Nagpal and Lane-Fall et al. had small sample sizes which may not be an adequate representation. Stahl et al. did not evaluate patient outcomes, but more so evaluated the incidence of sentinel safety events and other quality of care indicators. As with other studies it is difficult to conclude the clinical impact of the cumulative errors [19-22].
Quantitative analysis
A total of 4,688 and 4,775 patients were in the intervention and comparison groups respectively. Due to only 1 study being included for the outcomes of handoff and medical errors, we are unable to analyze these outcomes using meta-analysis, Table 2B.
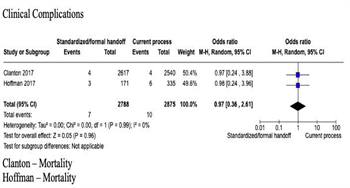
Clinical Complications:
While there were less reported clinical complications for the patients who received a standardized handoff, this did not reach significance in the pooled data (OR 0.97, 95% Confidence Interval 0.36, 2.61 p=0.96). Heterogeneity was low (I2<50%) which suggests that chance satisfactorily provides an explanation for the variability in the individual point estimates, Figure 2B.
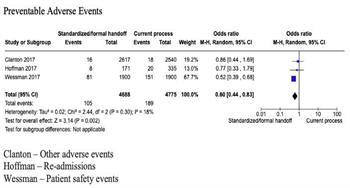
Preventable Adverse Events:
The pooled data demonstrates that patients who received a standardized handoff were less likely to experience preventable adverse events (OR 0.60, 95% Confidence Interval 0.44, 0.83 p=0.002). Again, heterogeneity was low (I2<50%) which suggests that chance satisfactorily provides an explanation for the variability in the individual point estimates, Figure 2B.
Grading the Evidence
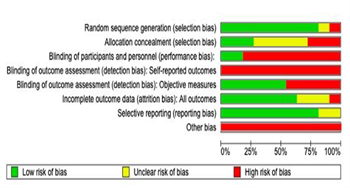
Among the studies included in our review, two were prospective, randomized, control studies [13][19], six were prospective cohort studies [4][13-15][20], two were retrospective cohort studies [18][21], and one was a case-control study [22]. The most common standardized handoff used was a checklist or other formal tool including verbal, written, and electronic forms. The studies included pre and post-implementation designs with observation and evaluation. There was variability of the methods of handoff utilized as well as the structure of the studies. In addition, the risk of bias was considered serious as the majority of the included studies were observational with a lack of blinding or randomization. The inconsistency, indirectness, and imprecision were considered not serious. Due to the small number of studies despite a positive association, publication bias was considered significant. The clinical impact of a handoff error or medical error is unclear, as most of the studies did not evaluate the clinical outcome, cost or impact at the patient level. Based on the above information, overall, the quality of evidence was very low across all outcomes. The Risk of Bias graph is summarized in Figures 3.
This systematic review has some limitations. The majority of the studies were observational with an apparent selection bias and observer bias. These studies demonstrate encouraging results in the field of ACS, specifically perioperative interactions and intra/inter floor and ICU interactions for handoffs and transitions of care with improved communication. At this time, it is difficult to make conclusions regarding EMS to trauma team handoffs outside of expert opinion due to the lack of studies that met inclusion criteria. This work emphasizes the need for further prospective evaluation of this high stakes transition of care for our ACS population. The studies took place in a single institution or unit with small sample sizes, both of which may affect generalizability. All of the studies involved a component of observation of the handoff process and possible Hawthorne effect whereby observer behavior is altered by the observation process. Each study structure consisted of pre and post-interventions, making determination of trends unrelated to institutional or environment effect difficult. The studies tried to minimize this by using observers not involved in the transformation process. The varying reporting of outcomes and their definitions made it difficult to compare the various studies and their interventions.
Recommendations
Based on the evidence, the majority voted in favor of the following recommendations, 93%, 64%, 54%, and 87% respectively. Despite the very low quality of evidence, the implementation of a standardized handoff is considered likely beneficial in the setting of ACS, specifically perioperative interactions, EMS and trauma team interactions, and intra/inter floor and ICU interactions. In addition, development and implementation of a standardized handoff takes into account an institution’s current state/processes to optimize pre-existing infrastructure as well as feedback after initial implementation. In order to enact long term change, a larger culture shift towards improved patient safety is required.
Based on the aforementioned group consensus and expert opinion, we conditionally recommend a standardized handoff in the field of ACS, including perioperative interactions, EMS and trauma team interactions, as well as intra-inter floor and ICU interactions. At this time, other clinical benefits such as complications and the ideal structure remain less clear. The recommendations are summarized on Table 3.
Using These guidelines in Clinical Practice
This systematic review and meta-analysis highlight the best available evidence pertaining handoffs and transitions of care in the ACS patient population including perioperative interactions, EMS and trauma team interactions, and intra/inter floor and ICU interactions. Handoffs occur multiple times during an ACS patient’s hospitalization and this review specifically evaluates the nuances of ACS transitions of care at the physician level.
The ACS patient population inherently adds a level of acuity to the care provided, making standardizing this communication important, and this handoff even more high risk. As mentioned above, standardization and formal handoff processes reduce the rate of handoff errors and preventable adverse events in perioperative interactions and intra/inter floor and ICU interactions for ACS. This suggests the various transitions of care an ACS patient experiences should be taught and formalized from admission to discharge. The EMS and receiving trauma team interactions have not been as well studied, but in practice it is clear that streamlined communication of key information for critically ill trauma patients cuts down on questions asked, helps the care team better understand a patient’s presentation, and likely decreases time to the next phase of care. When implementing or standardizing new processes, it is imperative to understand how the system works at one’s institution, tailor such transitions of care to improve the existing work flow, and gain buy-in from key stakeholders.
The paucity of high quality data precludes us from making strong recommendations for or against standardized handoffs at this time; however, this review provides an up to date summary of what is known in ACS transitions of care and where opportunities for further investigation exist. As there was variety in the standardized protocol used in each study, best practices remain to be determined. It is reasonable to conclude a succinct, standardized handoff tool that is used during each phase of an ACS patient’s hospitalization, would improve communication and as a by-product, potentially patient outcomes. This tool should include identifying patient details, their current state, treatment performed, information pending, and plans/next steps.
Future Directions
Future prospective, randomized trials investigating the clinical impact of standardized handoffs and transitions of care in ACS are needed to develop the recommended structure, the necessary elements, and to understand the impact this has on clinical outcomes of our patients.
References
- ^ Joint Commission on Accreditation of Healthcare Organizations. Sentinel Event Website. https://www.jointcommission.org/resources/sentinel-event/. Updated 2023.
- ^ Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001.
- ^ Ivatury RR, Guilford K, Malhotra AK, Duane T, Aboutanos M, Martin N. Patient Safety in Trauma: maximal impact management errors at a level I trauma center. J Trauma. 2008;64:265–272.
- ^ a b c d e Shah AC, Herstein AR, Flynn-O’Brein KT, Oh DC, X AH, Flanagan MR. Six Sigma Methodology and Postoperative Information Reporting: A Multidisciplinary Quality Improvement Study With Interrupted Time-Series Regression. J Surg Educ. 2019;76(4):1048-1067.
- ^ Catchpole KR, de Leval MR, McEwan A, Pigott N, Elliott MJ, and McQuillan A et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17(5):470–478.
- ^ Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med. 2011;12(3): 304–308.
- ^ a b Kerwin AJ, Haut ER, Burns JB, Como JJ, Haider A, and Stassen N et al. The Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. J Trauma. 2012;73(5 Suppl 4):S283-287.
- ^ Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. 2022. Available at covidence.org.
- ^ Review Manager (RevMan) [Computer program]. Version 5.4. The Cochrane Collaboration, 2020.
- ^ Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-58.
- ^ GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime, 2022. Available from gradepro.org.
- ^ a b c Nagpal K, Abboudi M, Manchanda C, Vats A, Sevdalis N, and Bicknell C. Improving postoperative handover: a prospective observational study. Am J Surg. 2013;206(4):494-501.
- ^ a b c Salzwedel C, Mai V, Punke MA, Kluge S, Reuter D. The effect of a checklist on the quality of patient handover from the operating room to the intensive care unit: A randomized controlled trial. J Crit Care. 2016;32:170-4.
- ^ a b Faiz T, Saeed B, Ali S, Abbas Q, Malik M. OR to ICU handoff: theory of change model for sustainable change in behavior. Asian Cardiovasc Thorac Ann. 2019;27(6):452-458.
- ^ a b Lane-Fall MB, Pascual JL, Peifer HG, Di Taranti LJ, Collard ML, and Jablonski J et al. A Partially Structured Postoperative Handoff Protocol Improves Communication in 2 Mixed Surgical Intensive Care Units: Findings From the Handoffs and Transitions of Critical Cre (HATRICC) Prospective Cohort Study. Ann Surg. 2020;271(3):484-493.
- ^ Nagpal K, Abboudi M, Fischler L, Schmidt T, Vats A, and Manchanda C et al. Evaluation of postoperative handover using a tool to assess information transfer and teamwork. Ann Surg. 2011;253(4):831-7.
- ^ Theory of Change. What is Theory of Change? https://www.theoryofchange.org/what-is-theory-of-change/. Updated 2023.
- ^ a b c d Talbot R, Bleetman A. Retention of information by emergency department staff at ambulance handover: do standardized approaches work?. Emerg Med J. 2007;24(8):539-42.
- ^ a b c Lee JC, Horst M, Rogers A, Rogers FB, Wu D, and Evans T et al. Checklist-styled daily sign-out rounds improve hospital throughput in a major trauma center. Am Surg. 2014;80(5):434-40.
- ^ a b Clanton J, Gardner A, Subichin M, McAlvanah P, Hardy W, and Shah A et al. Patient Hand-Off iNitiation and Evaluation (PHONE) study: A randomized trial of patient handoff methods. Am J Surg. 2017;213(2):299-306.
- ^ a b Hoffman RL, Saucier J, Dasani S, Collins T, Holena DN, and Fitzpatrick M et al. Development and implementation of a risk identification tool to facilitate critical care transitions for high-risk surgical patients. Int J Qual Health Care. 2017;29(3):412-419.
- ^ a b Wessman BT, Sona C, Schallom M. A Novel ICU Hand-Over Tool: The Glass Door of the Patient Room. J Intensive Care Med. 2017;32(8):514-519.
- Stahl K, Palileo A, Schulman CI, Wilson K, Augenstein J, and Kiffin C et al. Enhancing patient safety in the trauma/surgical intensive care unit. J Trauma. 2009;67(3):430-3.