Rectal Injuries, Penetrating Extraperitoneal (UPDATE IN PROCESS)
Published 2016
Citation: J Trauma. 80(3): 546–551, March 2016
Authors
Bosarge, Patrick L. MD; Como, John J. MD, MPH; Fox, Nicole MD; Falck-Ytter, Yngve MD; Haut, Elliott R. MD, PhD; Dorion, Heath A. MD; Patel, Nimitt J. MD; Rushing, Amy MD; Raff, Lauren A. MD; McDonald, Amy A. MD; Robinson, Bryce R.H. MD, MS; McGwin, Gerald Jr PhD; Gonzalez, Richard P. MD
Author Information
From the Departments of Surgery (P.L.B., L.A.R.), and Epidemiology (G.M.), University of Alabama at Birmingham, Birmingham, Alabama; Department of Surgery (J.J.C., N.J.P., A.A.M.), Metrohealth Medical Center, Case Western Reserve University; and Division of Gastroenterology (Y.F.-Y.), Case Western Reserve University, Case and VA Medical Center, Cleveland; Department of Surgery (H.A.D.), Mercy Health St. Elizabeth Youngstown Hospital, Youngstown; and Department of Surgery (A.R.), Ohio State University Wexner Medical Center, Columbus, Ohio; Department of Surgery (N.F.), Cooper University Health Care, Camden, New Jersey; Department of Surgery (E.R.H.), The Johns Hopkins Hospital, Baltimore, Maryland; Department of Surgery (B.R.H.R.), Harborview Medical Center, University of Washington, Seattle, Washington; and Department of Surgery (R.P.G.), Loyola University Medical Center, Maywood, Illinois.
Submitted: November 11, 2015, Accepted: December 4, 2015, Published online: December 26, 2015.
Address for reprints: Patrick L. Bosarge, MD, Division of Trauma, Burns, and Surgical Critical Care, University of Alabama, Birmingham, University of Alabama Medical Center, 112 Lyons-Harrison Research Bldg, 701 19th St South, Birmingham, AL 35294; email: pbosarge@uabmc.edu.
Objectives
The objective of this guideline was to evaluate the use of diversion, DRW, and PD in nondestructive penetrating extraperitoneal rectal injuries. The Population (P), Intervention (I), Comparator (C) and Outcome (O) questions were defined as follows:
PICO Question 1
In patients with nondestructive penetrating extraperitoneal rectal injuries (P), should proximal diversion (I) be performed versus no proximal diversion with primary repair (if feasible) (C) to decrease the incidence of complications (O)?
PICO Question 2
In patients with nondestructive penetrating extraperitoneal rectal injuries (P), should presacral drainage (I) versus no presacral drainage (C) be performed to decrease the incidence of complications (O)?
PICO Question 3
In patients with nondestructive penetrating extraperitoneal rectal injuries (P), should distal rectal washout be performed (I) versus no distal rectal washout (C) to decrease the incidence of complications (O)?
Identification of References
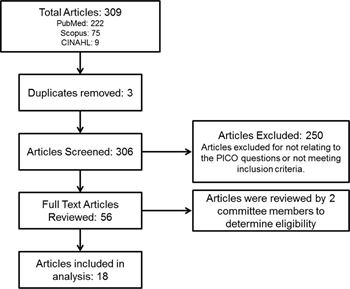
Figure 1. Study selection flow diagram.
With the assistance of a professional medical librarian, a search of the National Library of Medicine and the National Institutes of Health MEDLINE database was conducted using and IndexCat, as well as proprietary indices hosted by Elsevier (Scopus) and EBSCO (CINAHL) with citations published between January 1900 and July 2014. We used the “related articles” function to broaden the search and scan all citations for relevance. In addition to the electronic search, we manually searched the bibliographies of recent reviews and articles. Articles were limited to those in the English language involving human subjects. A systematic review of the available databases using , IndexCat, Scopus, and CINAHL was performed with the following search terms: rectum, rectal, anorectal, trauma, wound, injury, penetrating, firearm, gunshot, stab, impale, and human. Letters to the editor, single-case reports, book chapters, and review articles were excluded. Articles that focused specifically on injuries related to combat were excluded. In addition, pediatric literature was included in the search; however, none of the data addressed the PICO questions. Of the 306 articles identified, 250 were eliminated for not relating to the PICO questions or not meeting inclusion criteria. The remaining 56 articles were each reviewed by two committee members to determine eligibility in this review. This resulted in 18 articles meeting inclusion criteria and addressing the PICO questions that had been formulated to create these guidelines (Fig. 1).
Outcome Measure Types
As per the GRADE approach, outcomes were chosen by the committee and rated in importance from 1 to 9, with scores of 7 to 9 representing critical outcomes (Table 1). For all PICO questions, the following outcomes were considered by committee members: mortality, sepsis, intra-abdominal infection, postoperative intervention, fistula development, bleeding complications, stoma complications, soft tissue infection, incontinence, antibiotic timing, and antibiotic complications.
The outcomes deemed critical by vote of the committee included mortality, sepsis, and intra-abdominal infection. Unfortunately, sepsis and intra-abdominal infection were not uniformly delineated in the identified studies; thus, the committee combined these two outcomes into infectious complications. The remainder of the outcomes were considered not critical by the committee and were not used in the decision-making process.
Data Extraction and Methodology
Following identification of the potentially pertinent 56 articles, each article was assigned to two committee members for extraction of data for each PICO in question. Because of the small numbers reported as well as heterogeneity and variability in reporting of data among the articles, meta-analysis was not practical for this guideline. Of the articles that were identified, only two were prospective, one observational[1] and one randomized.[3]
PICO Question 1
Fourteen articles were identified which addressed PICO Question 1.[1][3–17] Data reported for mortality and infectious complications were pooled to determine overall rates. Intrinsic limitations of the data existed because of heterogeneity, nonstandardized study designs, and incomplete reporting of complications. In addition, several studies did not delineate between intraperitoneal and extraperitoneal injuries.
PICO Question 2
Seventeen articles were reviewed by the committee from which data were extracted to address PICO Question 2.[1][3–6][8–19] Similarly to PICO Question 1, data reported for the outcomes of mortality and infectious complications were pooled to determine overall rates. The same limitations seen with PICO Question 1 existed.
PICO Question 3
Thirteen articles were available to address PICO Question 3.[1][5–12][14–17] The data obtained for the outcomes of mortality and infectious complications were pooled to determine overall rates. This data set was limited similarly to the data for PICO Questions 1 and 2.
Results for Pico Question 1
In patients with nondestructive penetrating extraperitoneal injuries (P), should proximal diversion (I) be performed versus primary repair (if feasible) without proximal diversion (C) to decrease the incidence of infectious complications (O) (Table 2)?
Qualitative Synthesis
Proximal diversion has been considered the hallmark of management for penetrating rectal injuries since World War II. The literature comparing diversion versus nondiversion is significantly lacking in the present literature pool. Upon this review, 14 studies have taken into consideration the critical outcomes of mortality and infectious complications in the setting of proximal diversion. The nondiversion comparator group is quite small (26 patients) versus the diversion group (532 patients). Only one study was prospective in nature for this PICO, which had a small number of participants.[1] In that study, Gonzalez et al. assigned 14 patients to one of two algorithms for the treatment of nondestructive extraperitoneal rectal injuries, neither of which involved colostomy formation. No patient in the study had an infectious complication related to the rectal injury, and there was no mortality. This one study represents more than half of the patients (14 of 26) identified in the literature treated without colostomy for extraperitoneal rectal injuries. Overall, there is no reported mortality in the nondiversion group (0 of 26), while the diversion group has a mortality rate of 1.7% (9 of 523). Unfortunately, it is unclear as to whether death in these patients was specifically related to the complications of the rectal injury or is related to overall trauma burden to include hemorrhagic shock. Regarding the second critical outcome of infectious complications, the diversion group had nearly a 50% reduction (diversion, 8.8% vs. nondiversion, 18.2%) of overall infectious complications.
Quantitative Synthesis (Meta-analysis)
Meta-analysis was not appropriate because of the small numbers reported, as well as heterogeneity and variability in the reporting of data among the articles.
Grading the Evidence
The overwhelming majority of data related to this PICO question was retrospective and observational in nature. With the use of the GRADE framework for evaluating the data related to the outcomes of mortality and infectious complications, the quality of the data for this specific PICO question suffers because of risk of bias and imprecision. Bias was assigned because of the majority of the studies use historical controls. Imprecision was determined because of the very low numbers of events seen within the comparator group. Because of these factors, the overall quality of evidence has been determined to be very low.
Recommendation
Within the GRADE framework, once the overall quality of evidence across studies and outcomes is determined, the guideline panel formulates a recommendation that considers the following: quality of evidence, balance between desirable and undesirable outcomes, patients’ values and preferences, and cost/resource use. Despite the overall quality of evidence being very low, the panel considered that most patients would place a high value on avoidance of mortality and infectious complications. All of these factors resulted in the formulation of a conditional recommendation by the committee. The committee concludes that the desirable effects of adherence to a recommendation probably outweigh the undesirable effects. Thus, in patients with nondestructive penetrating extraperitoneal rectal injuries, we conditionally recommend proximal diversion (vs. nondiversion).
Results for Pico Question 2
In patients with nondestructive penetrating extraperitoneal rectal injuries (P), should presacral drainage (I) versus no presacral drainage (C) be performed to decrease incidence of infectious complications (O) (Table 3)?
Qualitative Synthesis
Advocated for the management of penetrating rectal injuries since World War II, the use of PD began to significantly decline after Gonzalez et al.[3] reported in a small, albeit important, randomized prospective study involving 50 patients randomized to two arms, of which the first was diversion and PD and the other was diversion and no PD. Two patients died of complications unrelated to the rectal injury. Therefore, 23 patients underwent PD, and 25 patients underwent no PD. There was no statistical difference in complications between the groups.
Upon formulation of this guideline, 17 studies have addressed the critical outcomes of mortality and infectious complications in the setting of presacral drainage. The no presacral drainage comparator group had a total of 267 patients versus the presacral drainage group of 395 patients. Overall mortality in the presacral drainage group was 1.77% versus 0.75% in the group without presacral drain. Similar to PICO Question 1, the pooled data are not clear as to whether death is specifically related to the management of the rectal injury or if death is related to overall trauma burden from associated injuries and hemorrhage, which seems likely. Regarding the second critical outcome of infectious complications, the no presacral drain group had a 40% reduction of overall infectious complications (no PD, 5.71% vs. PD, 9.63%).
Quantitative Synthesis (Meta-analysis)
Meta-analysis was not appropriate because of the small numbers reported, as well as heterogeneity and variability in the reporting of data among the articles.
Grading the Evidence
With the use of the GRADE framework for evaluating the data related to the outcomes of mortality and infectious complications, one randomized prospective study was specific to this PICO, question, which represented approximately 7% of the total pooled data, with the remainder of the data being retrospective and observational in nature. No serious inconsistency was detected; however, serious concerns for risk of bias and imprecision were noted among the representative studies. The inconsistency in study design and data reporting lowered the grade for this PICO. Therefore, the overall quality of evidence was considered very low by the committee.
Recommendation
In patients with nondestructive extraperitoneal rectal injuries, we conditionally recommend against the routine use of presacral drains.
Results for Pico Question 3
In patients with nondestructive penetrating extraperitoneal rectal injuries (P), should distal rectal washout be performed (I) versus no distal rectal washout (C) to decrease the incidence of infectious complications (O) (Table 4)?
Qualitative Synthesis
Distal washout of stool from the rectum after penetrating wounds is a historical staple of management for rectal injuries. Many clinicians today have eliminated this component of management from their practices. Thirteen studies were included to adjudicate this PICO question. The non-DRW comparator group contained 301 patients versus the DRW group of 202 patients. Mortality for the group non-DRW group was 1.37% versus 0.99% in the DRW group. Like all PICO questions, the data are not clear as to whether death was related to the rectal injury management or if death is related to overall trauma burden from associated injuries. The second critical outcome of infectious complications demonstrated no difference between the groups (non-DRW, 10.30% vs. DRW, 9.90%).
Quantitative Synthesis (Meta-analysis)
Meta-analysis was not appropriate because of the small numbers reported, as well as heterogeneity and variability in the reporting of data among the articles.
Grading the Evidence
With the use of the GRADE framework for evaluating the data related to the outcomes of mortality and infectious complications, there was only one prospective observational study for this PICO, and this article included small numbers of participants (14 patients) that were not managed with DRW, without a comparator group.[1] The overwhelming data related to this PICO question were retrospective and observational in nature. No serious risk of bias was detected; however, inconsistency among the studies in design and data reporting lowered the grade for this PICO question. Therefore, the overall quality of evidence was considered very low by the committee.
Recommendation
In patients with nondestructive penetrating extraperitoneal rectal injuries, we conditionally recommend not performing distal rectal washout (vs. performance of distal rectal washout).
Using These Guidelines in Clinical Practice
These guidelines represent a detailed summary and comprehensive overview of the literature regarding the evaluation and treatment of penetrating extraperitoneal rectal injuries. The literature available for review conditionally supports the use of proximal diversion for avoidance of infectious complications. Furthermore, the literature supports a conditional recommendation for not performing presacral drainage and distal rectal washout to avoid infectious complications. The recommendations are meant to inform the decision-making process and not replace clinical judgment as individual patient circumstances/conditions may dictate variation to the suggested recommendations. The data regarding mortality related to each PICO question are questionable to the committee because the raw reporting of mortality was overwhelmingly unaccompanied by explanation of the cause of death.
Conclusion
In summary, we propose three conditional evidence-based recommendations regarding the management of nondestructive extraperitoneal penetrating rectal injury in the non–combat-injured patient, which were formulated using the GRADE methodology. We conditionally recommend proximal diversion for management of these injuries. The committee conditionally recommends the avoidance of both routine presacral drains and distal rectal washout in the management of these injuries.
Authorship
P.L.B., J.J.C., and E.R.H. conceived of this study. P.L.B., J.J.C., H.A.D., R.P.G., E.R.H., A.A.M., N.J.P., L.A.R., and A.R. developed the PICO questions. P.L.B., J.J.C., H.A.D., N.F., R.P.G., A.A.M., N.J.P., L.A.R., and A.R. examined the literature. P.L.B., J.J.C., H.A.D., N.F., R.P.G., A.A.M., N.J.P., L.A.R., and A.R. performed the data extraction. P.L.B., J.J.C., H.A.D., Y.F.Y., N.F., R.P.G., E.R.H., A.A.M., G.M., N.J.P., L.A.R., and A.R. contributed to the data interpretation. P.L.B., J.J.C., Y.F.Y., N.F., and B.R. wrote the manuscript.
Acknowledgment
The Committee would like to thank Carolyn M. Holmes of the Lister Hill Library of the Health Sciences at the University of Alabama at Birmingham for the assistance in identifying all of the literature used to develop this practice management guideline.
The authors would also like to thank the Eastern Association for the Surgery of Trauma (EAST) and the EAST Foundation for the opportunity to write this article and the detail-oriented peer review of this article by the practice management guidelines section.
Disclosure
The authors declare no conflicts of interest.
References
- Gonzalez RP, Phelan H 3rd, Hassan M, Ellis CN, Rodning CB. Is fecal diversion necessary for nondestructive penetrating extraperitoneal rectal injuries? J Trauma. 2006; 61(4): 815–819.
- Pasquale M, Fabian TC. Practice management guidelines for trauma from the Eastern Association for the Surgery of Trauma. J Trauma. 1998; 44(6): 941–956.
- Gonzalez RP, Falimirski ME, Holevar MR. The role of presacral drainage in the management of penetrating rectal injuries. J Trauma. 1998; 45(4): 656–661.
- Bartizal JF, Boyd DR, Folk FA, Smith D, Lescher TC, Freeark RJ. A critical review of management of 392 colonic and rectal injuries. Dis Colon Rectum. 1974; 17(3): 313–318.
- Vitale GC, Richardson JD, Flint LM. Successful management of injuries to the extraperitoneal rectum. Am Surg. 1983; 49(3): 159–162.
- Mangiante EC, Graham AD, Fabian TC. Rectal gunshot wounds. Management of civilian injuries. Am Surg. 1986; 52(1): 37–40.
- Shannon FL, Moore EE, Moore FA, McCroskey BL. Value of distal colon washout in civilian rectal trauma–reducing gut bacterial translocation. J Trauma. 1988; 28(7): 989–994.
- Burch JM, Feliciano DV, Mattox KL. Colostomy and drainage for civilian rectal injuries: is that all? Ann Surg. 1989; 209(5): 600–610.
- Thomas DD, Levison MA, Dykstra BJ, Bender JS. Management of rectal injuries. Dogma versus practice. Am Surg. 1990; 56(8): 507–510.
- Ivatury RR, Licata J, Gunduz Y, Rao P, Stahl WM. Management options in penetrating rectal injuries. Am Surg. 1991; 57(1): 50–55.
- Bostick PJ, Johnson DA, Heard JF, Islas JT, Sims EH, Fleming AW, Sterling-Scott RP. Management of extraperitoneal rectal injuries. J Natl Med Assoc. 1993; 85(6): 460–463.
- Levy RD, Strauss P, Aladgem D, Degiannis E, Boffard KD, Saadia R. Extraperitoneal rectal gunshot injuries. J Trauma. 1995; 38(2): 273–277.
- Steinig JP, Boyd CR. Presacral drainage in penetrating extraperitoneal rectal injuries: is it necessary? Am Surg. 1996; 62(9): 765–767.
- Navsaria PH, Shaw JM, Zellweger R, Nicol AJ, Kahn D. Diagnostic laparoscopy and diverting sigmoid loop colostomy in the management of civilian extraperitoneal rectal gunshot injuries. Br J Surg. 2004; 91(4): 460–464.
- Shatnawi NJ, Bani-Hani KE. Management of civilian extraperitoneal rectal injuries. Asian J Surg. 2006; 29(1): 11–16.
- Navsaria PH, Edu S, Nicol AJ. Civilian extraperitoneal rectal gunshot wounds: surgical management made simpler. World J Surg. 2007; 31(6): 1345–1351.
- Ahmed N, Thekkeurumbil S, Mathavan V, Janzen M, Tasse J, Chung R. Simplified management of low-energy projectile extraperitoneal rectal injuries. J Trauma. 2009; 67(6): 1270–1271.
- McGrath V, Fabian TC, Croce MA, Minard G, Pritchard FE. Rectal trauma: management based on anatomic distinctions. Am Surg. 1998; 64(12): 1136–1141.
- Weinberg JA, Fabian TC, Magnotti LJ, Minard G, Bee TK, Edwards N, Claridge JA, Croce MA. Penetrating rectal trauma: management by anatomic distinction improves outcome. J Trauma. 2006; 60(3): 508–513.
Tables
|
Outcome |
Average |
Importance |
Include in GRADE Evidence Pro?le |
|
Mortality |
8.7 |
Critical |
Yes |
|
Sepsis |
8.3 |
Critical |
Yes |
|
Intra-abdominal infection |
7.8 |
Critical |
Yes |
|
Postoperative intervention |
6.1 |
Important |
No |
|
Fistula |
5.8 |
Important |
No |
|
Bleeding |
5.3 |
Important |
No |
|
Stoma complications |
4.8 |
Important |
No |
|
Soft tissue infection |
3.0 |
Less important |
No |
|
Incontinence |
3.0 |
Less important |
No |
|
Antibiotic length of time |
2.3 |
Less important |
No |
|
Antibiotic complications |
2.3 |
Less important |
No |
*Historical controls only.
**Inconsistency could not be adequately assessed.
†Few events; total patients enrolled in the intervention group low.‡No reliable relative comparative effect estimate available because of comparison with historical controls.
*Historical controls only.
**Inconsistency could not be adequately assessed.
†Few events; total patients enrolled in the intervention group low.
‡No reliable relative comparative effect estimate available because of comparison with historical controls.
?
*Historical controls only.
**Inconsistency could not be adequately assessed.
†Few events; total patients enrolled in the intervention group low.
‡No reliable relative comparative effect estimate available because of comparison with historical controls.